VITAMIN D
Vitamin D is a crucial nutrient that plays an essential role in our overall health and wellbeing. It is known for its critical functions in promoting bone health, but its benefits extend far beyond that. Recent studies have shown that Vitamin D also plays a significant role in boosting our immune system, protecting us against various infectious diseases, and promoting good mental health.
Despite the widespread awareness of the importance of Vitamin D, many people still suffer from its deficiency, which can lead to severe health consequences. In this long-form article, we will delve deeper into the benefits of Vitamin D on our immune system, infectious diseases, mental health, and bone health. We will explore the latest research and clinical trials on the topic, shedding light on the mechanisms through which Vitamin D exerts its positive effects on our health.
By the end of this article, you will have a thorough understanding of the importance of Vitamin D and how it can benefit your overall health and wellbeing.
Table of Contents
- Sources & Intake
- Synthesis from The Sun
- Structure
- Bioactivation
- Variants of Supplementation
- Target Levels
- Deficiency (Predictors)
- Supplementation
- Lifespan
- Neurology
- Cognition
- Depression
- Multiple Sclerosis
- Alzheimer’s
- Parkinson’s
- Sleep Quality
- Disease Risk
- Blood Pressure
- Cardiac Tissue
- Red Blood Cells
- Blood Flow
- Atherosclerosis
- Insulin Sensitivity
- Diabetes
- Fat Mass & Obesity
- Skeletal Muscle & Physical Performance
- Deficiency
- Performance
- Injury & Illness
- Skeleton & Bone Metabolism
- Inflammation & Immunology
- Interactions with Hormones
- Testosterone
- Estrogen
- Interactions with Cancer Metabolism
- Interactions with Lungs
- Interactions with Sexuality
- Pregnancy and Lactation
- Interactions with Various Disease States
- Nutrient Interactions
- Safety & Toxicity
- Summary
Sources & Intake
Vitamin D is an essential nutrient that was discovered shortly after Vitamins A, B (before the realization that Vitamin ‘B’ was not a single molecule), and Vitamin C. It was first discovered as a constituent of Cod Liver Oil and was referred to as the ‘anti-rachitic’ compound due to its ability to counteract rickets.
Food sources of vitamin D3 include:
- Milk, being the most common source of vitamin D in the USA which its consumption has trended downwards in recent decades.
- Cod liver oil at around 2.54-2.78mcg/mL; although labels would be more precise on a product-specific basis as some are lower than this estimate such as 33.5-172.3IU/mL. [1]
In 1997, the Recommended Dietary Allowance (RDA) for Vitamin D was established at 400IU (International Units), which is approximately equal to 10mcg of Vitamin D3. This dosage was deemed sufficient to lower the risk of rickets in children.
Despite the current definition of deficiency, the intake of 400IU of Vitamin D, while considered clinically deficient in modern definitions, remains adequate for the prevention of rickets.
Although the target intake of 400IU of Vitamin D is sufficient to prevent rickets, it is widely regarded as inadequate for adults. Studies indicate that this dosage does not maintain circulating Vitamin D levels within the ideal range of 50-75nmol/L, which is considered optimal for good health. [1]
Main Takeaway: Dairy appears to be the best food source for vitamin D3. Cod liver oil effectiveness varies, depending on the processor and the method of analysis. While the previous Recommended Dietary Allowance (RDA) for Vitamin D was adequate to prevent rickets in children, it is now considered insufficient for adults. Research suggests that higher levels of Vitamin D intake are necessary to maintain optimal health in adults.
Synthesis from The Sun
Vitamin D synthesis can occur naturally when the skin is exposed to sunlight. This process involves the conversion of 7-dehydrocholesterol, a derivative of cholesterol stored in the body, into cholecalciferol, also known as Vitamin D3.
In some scenarios, the rate of vitamin D synthesis is reduced, such as:
- Regions further away from the equator tend to have lower rates of Vitamin D synthesis due to reduced exposure to solar radiation. Studies have shown that the Northern United States receives less UVB radiation compared to the Southern United States, which has been linked to an increased risk of cancer.
- Environmental factors such as cloudy weather or seasons with reduced daylight hours can also decrease solar exposure and, therefore, inhibit Vitamin D synthesis. [1]
- A combination of latitude and season, with the Northern Hemisphere (Boston and Edmonton; latitude 42.2-55°N) failing to produce any vitamin D between October and March.
- Regions with higher levels of ozone breakdown, measured by Dobson units, tend to have higher levels of UVB radiation.
- Darker skin has a slower synthesis rate than lighter skin and Black persons are routinely at a higher risk for vitamin D deficiency when compared to lighter skin tones (Asian, Caucasian, Hispanic) when other factors are controlled for. [1]
While some studies suggest that using sunscreen may reduce the risk of skin cancer such as Melanoma, [1] the results are mixed. Sunscreens appear to significantly hinder the synthesis of Vitamin D by interfering with the topical effects of UVB rays. [1] Chronic (not acute) sunscreen usage has been associated with Vitamin D deficiency.
Main Takeaway: Various factors such as latitude, skin tone, and environmental conditions can affect the rate of Vitamin D synthesis from sunlight. Of these factors, latitude and skin tone appear to be the most influential.
Those living closer to the equator have a greater ability to produce Vitamin D through sunlight exposure, while individuals with darker skin tones are at a higher risk of Vitamin D deficiency. In fact, it has been observed that areas located above latitude 42.2°N, such as Boston, fail to produce any UVB-induced previtamin D from November to February, a period of four months. This deficiency in Vitamin D synthesis is further prolonged to six months above latitude 55°N, as observed in Edmonton. However, regions located within the range of 18-32°N still produce Vitamin D during the winter.
Sunscreen is able to significantly diminish synthesis of vitamin D, and chronic usage may be associated with vitamin D deficiency, if no oral supplementation exists.
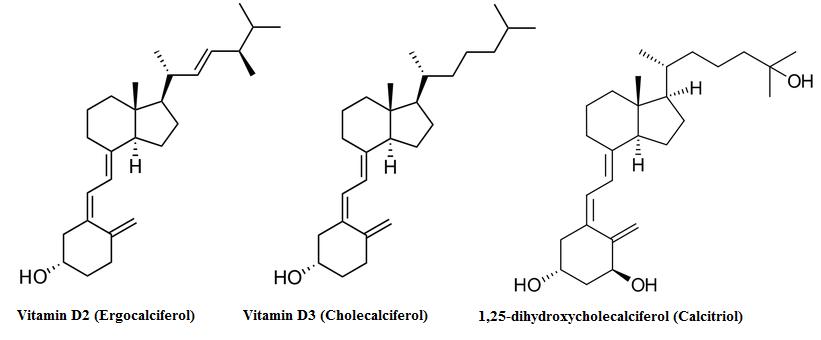
Structure
Vitamin D3, also called cholecalciferol, is the common supplement for vitamin D. It is better absorbed compared to other forms of vitamin D. In the liver, cholecalciferol is converted to 25-hydroxycholecalciferol by cholecalciferol 25-hydroxylase enzyme. The converted form is then transported to the kidneys where it is further hydroxylated into 1,25-dihydroxycalciferol, also known as Calcitriol. Calcitriol is the active hormone produced as a result of vitamin D3 ingestion.
Bioactivation
Vitamin D is classified as a steroid precursor, meaning that it is not active on its own and requires metabolic conversion to become active in the body. The body can obtain vitamin D through various pathways, including oral supplementation and biological synthesis in the skin.
In cases where oral supplementation is not necessary, the body must convert bodily stores of 7-dehydrocholecalciferol to cholecalciferol (Vitamin D3). This initial metabolite is naturally present in the skin and is activated by light (specifically, a spectrum of 280-320 nm UVB), which breaks down a component of the molecule called the B-ring. The metabolite, called pre-vitamin D3, then isomerizes to Vitamin D3 and can then be subject to metabolism in the liver. [1]
The process of converting cholecalciferol to 25-hydroxycholecalciferol involves the activity of a 25-hydroxylase enzyme, which can be mediated by either CYP2R1 or CYP27A1. The bioactivation process of cholecalciferol into 25-hydroxycholecalciferol is mainly carried out in the liver, with the involvement of the 25-hydroxylase enzyme, where both CYP2R1 and CYP27A1 enzymes play a role. The next enzyme in the process, CYP27B1, is primarily expressed in the kidneys. Therefore, a large amount of 25-hydroxycholecalciferol is released into the bloodstream to reach the kidneys. Once subjected to CYP27B1, the product is converted into 1,25-dihydroxycholecalciferol, which is considered the active form of Vitamin D as a hormone.
Main Takeaway: The activation of Vitamin D3 into its hormone form involves either two stages (if starting from a dietary supplement containing Vitamin D3) or three stages (if starting from skin stores). The skin initiates the first (non-supplemental) conversion, while the liver and kidneys mediate the later two metabolic steps.
Variants of Supplementation
Vitamin D is classified into two forms: ergocalciferol (vitamin D2) which is primarily obtained from plant sources and cholecalciferol (vitamin D3) which is produced by mammals and fish, making it a component of cod liver oil supplementation along with vitamin A and fish oil fatty acids. [1] The only difference in these two molecules is a methyl group, as vitamin D3 is 27 carbons in length, while D2 is 28 carbons.
Both vitamin D2 and D3 are seen as prohormone compounds (acting to increase circulating levels of 25-hydroxyvitamin D). There is ongoing debate about the superiority of the two forms of vitamin D, ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3), in increasing circulating 25-hydroxyvitamin D levels. Many experts suggest that vitamin D3 is more effective since the active hormone is 25-hydroxycholecalciferol and D2 is structurally more similar to D3 than D2. Some sources recommend against the sale of D2 as a supplement.
Some studies, such as 11 weeks of supplementation at the winter at 1,000IU (D2 or D3, with a third group given 500IU of each) either as supplementation or orange juice fortification have noted equivalence between the two forms, and elsewhere supplementation of 1,000IU daily in vitamin D deficient persons has noted a difference in circulating hormone levels but no differences in parathyroid hormone.
Other studies using daily dosing of 1,600IU for a year, 4,000IU over 14 days, of 50,000IU monthly doses for a year a one time dose as well as acute doses of up to 300,000IU D3 have also been noted to be more effective than D2.
According to a meta-analysis the difference in efficacy between D3 and D2 is more notable with bolus supplementation than with daily supplementation.
D2 is synthetically produced (for the purpose of supplementation) from irradiation of ergosterol (from mold ergot) whereas D3 is synthesized from 7-dehydrocholesterol. D2 appears to be less chemically stable than D3 ex vivo (not in an oil base, however) [1] leading to some authors suggesting that it may have a poorer shelf-life.
Main Takeaway:
Both vitamin D2 and D3 can be used as supplements to increase circulating levels of the active hormone. While some studies suggest that D3 is more effective than D2, others argue that the potency difference can be normalized by standardizing to an IU value.
There is conflicting evidence regarding the effectiveness of vitamin D2 and D3 when compared on an IU basis. Some studies have found them to be bioequivalent, while others suggest a superiority of vitamin D3. However, there are no studies suggesting that D2 is more effective than D3. As a result, it is recommended to choose D3 supplementation.
There are differences in the synthesis and stability of D2 and D3, which are two forms of vitamin D used for supplementation. D3 is synthesized differently from D2 and is more stable than D2 in powder form.
Target Levels
The generally accepted terms to refer to different possible ‘states’ of Vitamin D status are:
- Deficiency (Less than 30nmol/L or 12ng/mL, leading to rickets in children and osteomalacia in adults)
- Insufficiency (between 30-50nmol/L, the range of 12-20ng/mL)
- Adequate (between 50-125nmol/L, or 20-50ng/mL)
- High (above 125nmol/L or 50ng/mL) where 2.5 nmol/L is approximately equal to 1 ng/mL, and 1 microgram (mcg or µg) of Vitamin D3 is approximately 40IU.
A target of 75nmol/L has been considered to as optimal for bone health in older individuals and bone-related conditions such as dental health or reducing the risk of falls and fractures in the elderly. This also appears to be a target for colorectal cancer prevention. Even in studies that recommend higher oral intakes (5,000IU), the end goal still appears to be around 75-80nmol/L.
Main Takeaway: Recommended levels of vitamin D are roughly 75nmol/L (30ng/mL) for some conditions.
Deficiency (Predictors)
From 1988 onwards, there was an increase in the prevalence of vitamin D deficiency, with the percentage of the population below the 75nmol/L cut-off increasing from 55% to 77% in 2004. It appears to have somewhat stabilized, with 79% of the population below 80nmol/L.
Using other cut-offs, in 2010 29% of the American population was below 50nmol/L (clinical insufficiency) and 3% below 20nmol/L (clinical deficiency).
Seasonal variation can impact vitamin D levels, with lower levels observed at the end of winter compared to the end of summer. For instance, in Boston, which is located at latitude 42°N, 11% of people have vitamin D levels below 50nmol/L at the end of summer, while this number increases to 30% at the end of winter.
In a region that is slightly more northern on the other side of the world (Britain, latitude 53.1°N), rates of vitamin D deficiency still increase. At the end of summer, the percentage of the population having less than 25, 50, and 75nmol/L serum levels is 3.2%, 15.4%, and 60.9%, respectively. However, these values increase to 15.5%, 46.6%, and 87.1%, respectively, at the end of winter.
Estonia (59°N) has the percent of the population scoring below 25nmol/L and 50nmol/L recorded at 8% and 73% at the end of winter, respectively.
Even locations closer to the equator can experience vitamin D deficiency. For instance, in a study conducted in Isfahan City, Iran (located at 32°N), the percentages of the population recorded as having serum levels below 25, 50, and 75nmol/L were 26.9%, 50.8%, and 70.4%, respectively.
A potential confounding factor in the study conducted in Isfahan City, Iran is cultural and religious practices, as the population included both sexes, including women who wear religious clothing in public in this region. In Southern Florida (Miami, 25°N), 38% of men and 40% of women have been recorded as having serum levels below 50nmol/L.
Despite the above importance on latitude, at least one study has suggested that this may only account for one fifth of the variance seen.
One study found that deficiency is prevalent among medical inpatients, with 22% of patients having serum levels below 20 nmol/L and 57% having levels below 37.5 nmol/L.
In studies that divide populations into quartiles based on circulating vitamin D levels, it has been found that 50.3% of African Americans are in the lowest quartile (below 17.3 ng/mL in one study) while only 7.8% are in the highest quartile (32.1%). In comparison, white people had 9.5% in the lowest quartile and 43.5% in the highest quartile. Mexican-Americans and all other races were divided approximately 20% in each quartile. These results suggest the reduced synthesis rates of vitamin D associated with darker skin hold practical relevance.
Main Takeaway: Deficiency rates in the population appear to have increased over the past two decades but they may have stabilized in recent years.
Although latitude is a significant factor, it is important to note that vitamin D deficiency (defined by serum levels of 25nmol/L or below) and insufficiency (50nmol/L), are prevalent globally.
Supplementation
Approximately 1000IU daily is needed for 50% of the population to reach 75nmol/L, with 1700IU needed for 95% of the population to reach 75nmol/L.
Although the recommended daily doses for vitamin D are lower, studies have shown that the human body can metabolize higher amounts, such as 3000-5000 IU in men. Additionally, when the UV index is greater than 3, the body stops synthesizing vitamin D from sunlight at a level close to 10,000 IU.
A meta-analysis consisting of 76 trials was conducted to determine the effect of vitamin D supplementation on serum vitamin D levels in people over 50 years of age. The trials involved variable daily doses of vitamin D, ranging from 5-53.5mcg in most trials, with two trials using 124-250mcg daily or 225mcg. The trials were divided based on the amount of vitamin D that was supplemented. The analysis showed that supplementing with 10mcg was associated with an average increase of 9ng/mL in serum vitamin D levels, with an interquartile range (IQR; 25th-75th percentile) of 7.2-14.8ng/mL. Doubling the oral dose to 20mcg was associated with an average increase of 12.9ng/mL in serum vitamin D levels, with an IQR of 9.2-20.4ng/mL.
Similar results have been noted with another review noting that 100IU of Vitamin D3 increases serum Vitamin D by 1-2nmol/L and an increase of 10-25nmol/L with 1,000IU. Despite the first meta-analysis only being conducted in people over 50, this general dose-response over a period of time appears to exist for all age groups. [1, 2, 3]
Vitamin D was found to be best absorbed with a low-fat (11 g of fat) meal compared with both a high-fat (35 g of fat) meal and no meal.
The same research team conducted additional studies and discovered that fat plays a crucial role in increasing the absorption of vitamin D. Participants who consumed a meal containing 30 g of fat had peak vitamin D plasma levels that were 32% higher than those who consumed a fat-free meal with a similar protein content. The type of fat (polyunsaturated versus monounsaturated) did not appear to have an impact on absorption.
20,000IU daily has been associated with toxicity, while daily supplementation of 10,000IU does not appear to induce toxicity.
Sometimes acute boluses are used on a weekly or monthly basis, and toxicity has been associated with a bolus of 300,000IU.
Preloading a large bolus of Vitamin D, at 50,000-100,000IU, prior to a maintenance period does not appear to provide more benefit than simply taking a daily maintaining dose.
A meta-analysis comparing vitamin D2 and D3 found that when dosages were controlled on a weight basis (micrograms instead of IU), vitamin D3 resulted in a higher average increase in serum levels, with a difference of 4.29ng/mL compared to vitamin D2.
Main Takeaway: In general, a dose of 2,000 IU is sufficient to fulfill the vitamin D needs of most individuals. Doses ranging from 2,000-10,000 IU may not provide any additional benefits, but are not considered toxic either.
Regarding dosing, lower oral doses appear to be more effective in increasing serum vitamin D levels than higher doses, which may have reduced absorption. This variability between individuals suggests that different doses may be needed to achieve the desired level of serum vitamin D. At lower ranges of oral dosing, vitamin D seems to have a linear effect on serum levels, with each 100IU increasing serum by approximately 1-2nmol/L. For instance, 1,000IU is implicated in the range of 10-25nmol/L and 2,000IU in the range of 20-50nmol/L.
Vitamin D is best absorbed with a meal, preferrably one with a little fat in it.
Toxicity has been noted at very high daily doses of vitamin D, which are about 10-fold higher than the aforementioned 2,000IU daily dose.
Vitamin D3 appears to be a more reliable form of supplemental vitamin D, relative to D2, for increasing serum levels to an adequate range.
Lifespan & Extension
Low vitamin D levels are independently associated with an increase in all-cause mortality in the general population. Smaller samples sizes suggest that this association with mortality is not influenced by gender or by race, and is only dependent on circulating levels of vitamin D, although the higher frequency of low serum vitamin D in blacks (due to less skin synthesis rates) has been shown to increase the overall risk of mortality in an elderly cohort.
When comparing the lower circulating levels of vitamin D against the higher circulating levels in cohort studies, a relationship between risk of death and lower circulating levels are seen. [1, 2] It appears that the most benefit against mortality from vitamin D supplementation is a reduction in frailty of the elderly. [1]
According to some estimates, taking a daily dose of 1,000 IU vitamin D3, which is considered a lower dose, could reduce the medical costs associated with cancer treatment by approximately $16-$25 billion due to its potential protective and preventive effects.
Main Takeaway: Several observational studies have reported a negative association between serum vitamin D levels and all-cause mortality.
Clinical trials investigating the impact of vitamin D supplementation on mortality rates have suggested a small reduction in all-cause mortality, particularly in older adults.
Vitamin D3 supplementation appears to be the most efficient form of supplementation for reducing mortality.
It is possible that vitamin D might serve as a biomarker for another factor that is related to longevity. However, there is currently no evidence to suggest that vitamin D supplementation can increase lifespan directly. Rather, it appears that supplementation may indirectly reduce the risk of premature death.
Neurology
The enzyme needed to activate vitamin D appears to be expressed by neurons in the brain, with the hypothalamus and dopaminergic neurons of the substantia nigra having the highest concentrations of this enzyme. Most cells express the Vitamin D Receptor (VDR), but it appears to be absent in the nucelar basalis of Meynert and Purkinje cells in the cerebellum and is expressed in glial cells of the brain.
Calcium metabolism appears to **underlie neuronal cell death via excitotoxicity** [1, 2, 3] and hormonally active vitamin D confers a protective effect _in vitro_ at physiologically relevant concentrations up to 100nM but not above. This mechanism of protection appears to be mediated via a downregulation of L-type voltage-sensitive Ca2+ ion channels, an effect which has also been seen in bone cells. [1] These L-type channels have been implicated in excitotoxicity. [1]
A study conducted on rodents has observed that vitamin D has neuroprotective effects in vivo. The study noted that long-term treatment with vitamin D resulted in a slower rate of decline in neuronal density in the hippocampus during aging, which indicates the preservation of neuronal cells.
Main Takeaway: In vitro and animal data suggest that vitamin D can modulate a subset of calcium channels on neurons and regulate cell death through excitotoxicity.
Cognition
In vitamin D-sufficient young adults, the addition of 5000 IU vitamin D to the diet for one month failed to influence working memory, response inhibition, or cognitive flexibility despite serum levels of vitamin D being increased to an average 39 ng/mL. Anxiety and anger ratings were similarily unaffected.
However, an 18-week intervention in healthy adults reported that supplementing 4000 IU of vitamin D significantly improved visual memory but not verbal memory, executive function, or working memory. Average vitamin D levels were increased from 25 ng/mL to 52 ng/mL.
Depression
The relationship between vitamin D and depression was first reported in 1979, showing an inverse correlation between lower vitamin D status and more depressive symptoms. This association has resurfaced in populations at risk for cardiovascular incidents, fibromyalgia and in women during the winter.
Although some studies have found a correlation between vitamin D levels and depressive symptoms, the efficacy of vitamin D supplementation in treating depression is unclear and results have been inconsistent. [1, 2, 3, 4]
The potential benefits of vitamin D supplementation in alleviating depression symptoms appear to be greater in populations with preexisting low vitamin D levels.
Main Takeaway: There is evidence of an inverse relationship between vitamin D levels in the blood and symptoms of depression in certain groups.
Multiple Sclerosis
Multiple Sclerosis (MS) prevalence is **correlated with latitude and sun exposure**, [1, 2, 3]
both of which are in turn correlated with vitamin D levels. Vitamin D also appears to exert protective effects in an animal model of multiple sclerosis. [1, 2, 3]
Alzheimer's
There does appear to be some, albeit weaker, correlation between Alzheimer’s disease and vitamin D. [1, 2, 3, 4, 5] Vitamin D has been found to stimulate immune cells to catabolize amyloid-β protein aggregates in vitro.
Parkinson's
Low serum vitamin D is correlated with increased risk of Parkinson’s Disease (PD) and further associated with the severity of the disease state. [1, 2, 3, 4, 5, 6]
Vitamin D may have a neuroprotective effect on neurons under stress, [1] although a deficiency in vitamin D does not seem to necessarily increase the risk of neuronal damage in the cells linked to Parkinson’s disease. [1, 2]
Sleep Quality
Limited evidence suggests that a deficiency in vitamin D may have a negative impact on sleep quality, and increasing vitamin D levels may improve sleep function. [1, 2] However, further research is needed to confirm this relationship.
Disease Risk
Observational studies have indicated that low vitamin D levels are linked to an increased risk of cardiovascular disease.
Some clinical trials have suggested that vitamin D supplementation at moderate to high doses may reduce the risk of cardiovascular disease, although not all studies have found such an effect. [1]
Blood Pressure
Vitamin D has been shown to have a negative effect on renin expression, which in turn reduces the activity of the Renin-Angiotensin System (RAS). When there is a deficiency of vitamin D, the suppression of the RAS system is decreased, resulting in increased activity, which may subsequently raise blood pressure. [1, 2]
While vitamin D supplementation in humans has been associated with a slight reduction in blood pressure, the magnitude of this effect is weak, [1] and its efficacy may depend on metabolic alterations that cause hypertension. Nonetheless, in some individuals with hypertension, vitamin D supplementation may result in a small decrease in blood pressure.
Cardiac Tissue
Mice lacking the vitamin D receptor appear to have cardiac enlargement due to increased serum angiotension II and increased activity of the RAS system. [1, 2, 3]
Red Blood Cells
Supplementation with 800 IU vitamin D for 12 weeks in people with low vitamin D status but who were otherwise healthy led to small drops in red blood cell count, hemoglobin, and hematocrit when compared to placebo.
Blood Flow
Vitamin D status is associated with arterial stifness and vascular dysfunction in otherwise healthy humans.
Vitamin D levels have been associated with brachial flow-mediated dilation in Type 2 Diabetics. This indicates it plays an important role in heart function, especially in people with disease states.
Vitamin D status might in part help explain the difference in risk of the development of peripheral arterial disease in darker populations (who are more likely to be Vitamin D deficient).
Supplementing 3320IU/d of Vitamin D helped improve several health markers of cardiovascular health during weight loss.
Atherosclerosis
Vitamin D has been found to have a potential role in suppressing atherosclerosis by reducing oxidation in macrophages, a type of immune cell, at the endoplasmic reticulum (ER) level. [1]
When the ER is under stress, lipids and cholesterol can accumulate, leading to the formation of macrophages and foam cells, which contribute to plaque development. Vitamin D may attenuate this process.
Insulin Sensitivity
Vitamin D levels have been inversely correlated with insulin resistance and insulin sensitivity in non-diabetic adults and with serum levels of insulin in adolescents in the United States. There’s also an inverse correlation with insulin resistance in both obese and non-obese children.
Those considered to have insufficient levels of Vitamin D (50nmol/L or less) are more likely to be insulin resistant and have beta cell dysfunction than those who have higher levels of serum Vitamin D. Supplementation of Vitamin D has been found to improve insulin sensitivity in people who were found to be deficient in Vitamin D, and improve their tolerance to a glucose tolerance test.
In a randomized, controlled clinical trial high-dose vitamin D supplementation was shown to improve markers for glucose homeostasis in individuals with major depressive disorder (MDD).
Diabetes
Decreased serum Vitamin D levels increase risk of the development of Diabetes and with complications of Type 1 Diabetes. Higher Vitamin D levels prevent the occurence of Type 2 Diabetes and Vitamin D supplementation improves outcomes of Type 2 Diabetes.
Fat Mass & Obesity
Some studies have reported an association between low vitamin D levels and obesity, [1, 2, 3] but the reasoning is somewhat strained and dependent on caloric overconsumption. An association between lower vitamin D status and obesity has been noted in numerous trials. [1, 2, 3]
There is either no significant effect on fat mass overall or a possible pro-obesogenic effect associated with vitamin D supplementation at high doses. There is a very small amount of literature investigating this.
Skeletal Muscle & Physical Performance
There may not be any detectable vitamin D receptors on skeletal muscle tissue, despite a series of studies that suggest this. [1, 2, 3, 4, 5] Any suggesting findings appear to be caused by inprecise immunostaining techniques.
Despite the lack of vitamin D receptor expression directly on skeletal muscle cells, there appear to be impairments to physical function and reduced skeletal muscle hypertrophy associated with Vitamin D Receptor (VDR) knockout mice. [1, 2]
Deficiency
In vitro evidence suggests that vitamin D may improve muscle recovery after mechanical damage. A deficiency of Vitamin D is associated with an increase level of fat in skeletal muscle tissue in otherwise healthy young women. In young females, normalizing a Vitamin D deficiency does not appear to confer benefits to hand-grip or pinch-grip strength.
Performance
Supplementation of Vitamin D to correct a deficiency may improve Athletic performance in athletes. A serum Vitamin D level of 50ng/ml (125nmol/L) may be required to do so.
Daily supplementation of 4000IU of vitamin D on sedentary overweight/obese adults in conjunction with a resistance training program noted an increase in power output compared to placebo.
Another intervention on healthy young men found that 4000 IU of vitamin D daily for 6 weeks led to improved muscle recovery after damage induced by eccentric exercise of the quadriceps.
Injury & Illness
When assuming an optimal level of 75nmol/L, one study in NFL players noted that up to 64% of athletes had deficient Vitamin D levels, with a correlation existing between players getting injured having less Vitamin D levels. Vitamin D deficiency appears to be correlated with increased risk of illness and injury among athletes, especially in regards to stress fractures.
Main Takeaway: Daily supplementation of 4000IU appears to lead to improved performance in athletes along with muscle recovery after damage induced by eccentric exercise. A correlation between low Vitamin D levels, illness and athletic injuries appears to exist, especially in regards to stress fractures.
Skeleton & Bone Metabolism
Vitamin D acting upon its receptor does promote mineralization of bone tissue.
When examining stress fractures in youth, vitamin D is correlated with less risk for fractures. [1] Interventions of vitamin D supplementation appear to further protect individuals from stress fractures. Trials in elderly indivudals measuring fracture rates have noted a decreased rate in persons with Parkinson’s Disease with injections of active vitamin D hormone.
Supplementation of vitamin D appears to reduce the risk of falls in the elderly, but may only work in people with lower serum vitamin D levels at baseline. [1]
Serum vitamin D does not appear to correlate with osteoarthritic symptom presence or symptom severity or to significantly reduce joint pain associated with osteoarthritis
Inflammation & Immunology
Atopic Dermatitis, an inflammatory disease associated with dry, itchy skin, has been linked to Vitamin D deficiency. Numerous trials have demonstrated an association between Vitamin D supplementation and reduced symptoms of atopic dermatitis (AD), indicating that it may be a useful treatment option. However, while vitamin D has been deemed safe and effective for alleviating AD symptoms, it does not represent a cure for the condition.
Interactions with Hormones
Serum parathyroid hormone levels are inversely associated with Vitamin D until Vitamin D levels reach between 75 and 100 nmol/L, meaning serum levels below 75 nmol/L might indicate deficient levels of Vitamin D.
Testosterone
Vitamin D in serum appears to be positively correlated with overall androgen status, with sufficient levels of vitamin D acting to normalize testosterone. There is currently no evidence to suggest supraphysiological levels of vitamin D further enhances testosterone.
Estrogen
Vitamin D appears to regulate estrogen through the activity of the aromatase enzyme, which converts androgens into estrogens. Deletion of the vitamin D receptor in mice has been found to reduce aromatase activity, but calcium supplementation can alleviate this suppression, suggesting that Vitamin D regulates aromatase activity via calcium metabolism.
This study in receptor deficient mice noted reduced estrogen levels in serum, Follicle-Stimulating Hormone (FSH) to be increased in mice lacking the Vitamin D receptor, and this appears to be independent of calcium metabolism. Vitamin D also appears to be involved with Luteinizing Hormone (LH), as mice lacking the Vitamin D receptor (abolishing the effects of Vitamin D) appear to have elevated levels of LH.
Interactions with Cancer Metabolism
Vitamin D in serum appears to be inversely related to breast cancer risk (higher serum levels being associated with lower risk). [1] Furthermore, Vitamin D deficiency appears to be more prevalent in persons with diagnosed breast cancer [1] and is similarly correlated with severity of breast cancer. This risk appears more prevalent in black women, where one survey suggested 42% of black women in the US had serum levels below 15ng/mL (deficiency).
Supplemental ingestion of 400-800IU daily appears to be inadequate to decrease the risk of breast cancer. [1] Women supplementing with 2000IU of Vitamin D daily, may see up to a 50% reduction in the incidence of breast cancer.
Another study noted that while 1000IU daily was somewhat effective in improving Vitamin D status, a weekly administration of 50,000IU was more effective.
Vitamin D appears to be inversely correlated with risk of colon and colorectal cancers as well as with Prostate and Ovarian cancer.
For colorectal cancer outcomes, people with serum levels of 82.5 nmol/L or greater had a 50% lower risk of developing cancer than those with a serum level below 30 nmol/L, and this risk reduction was observed with 2000IU supplemental Vitamin D.
Doses as low as 600IU/d lower the risk of pancreatic cancer.
UVB irradiation (which produces Vitamin D) is associated with a decreased risk of developing ovarian cancer in women.
Main Takeaway: Vitamin D in serum appears to be inversely related to breast cancer risk (higher serum levels being associated with lower risk).
Furthermore, Vitamin D deficiency appears to be more prevalent in persons with diagnosed breast cancer and is similarly correlated with severity of breast cancer. 400-800IU daily appears to be inadequate to decrease the risk of breast cancer, whereas women supplementing with 2000IU of Vitamin D daily, may see up to a 50% reduction in the incidence of breast cancer.
Evidence suggests that even though 1000IU per day is somewhat effective in improving Vitamin D status, a weekly administration of 50,000IU is more effective.
Vitamin D appears to be inversely correlated with risk of colon and colorectal cancers, as well as with Prostate and Ovarian cancer.
For colorectal cancer outcomes, a reduction was observed with 2000IU of supplemental Vitamin D. Additionally, doses as low as 600IU/d lower the risk of pancreatic cancer.
Interactions with Lungs
In otherwise healthy adults, higher serum Vitamin D appears to be associated with improved lung function as assessed by forced exhalation. Low levels of Vitamin D are associated with increased corticosteroid use in asthmatic children, while supplementation of 1200IU daily is associated with decreased asthmatic attacks in children previously diagnosed with Asthma.
A study conducted in Japan noted that children taking 1200IU of Vitamin D daily were 40% less likely to get the flu during the winter while a Mongolian study on children and 300IU daily noted similar benefits. Supplementing with Vitamin D helps prevent the flu.
Vitamin D appears to be correlated with sleep quality.
Main Takeaway: Higher serum Vitamin D appears to be associated with improved lung function as assessed by forced exhalation.
Low levels of Vitamin D are associated with increased corticosteroid use in asthmatic children while supplementation of 1200IU daily is associated with decreased asthmatic attacks in children previously diagnosed with Asthma.
Children taking 1200IU of Vitamin D daily are 40% less likely to get the flu during the winter and supplementing with Vitamin D will help prevent the flu on adults.
Vitamin D also appears to be correlated with sleep quality.
Interactions with Sexuality
Mechanistically, vitamin D appears to act on the sperm itself (mature spermatid) and improve its motility while enhancing cell survival. [1, 2]
25-50ng/mL (62.4-124.8nmol/L) appears to be an adequate range to preserve optimal seminal properties in otherwise healthy men, with both lower and higher serum ranges being associated with infertility.
Pregnancy & Lactation
Research suggests that pregnant women have lower serum vitamin D levels compared to non-pregnant women, [1] and this deficiency can have adverse effects on both the mother [1] and the child. [1, 2] The deficiency is particularly critical during the first trimester, and therefore, supplementing vitamin D only after pregnancy notification may not be the best approach as it may miss the time-sensitive period.
A slightly higher intake of vitamin D may be required to reach sufficiency in pregnant women, relative to nonpregnant women and men, with intakes of up to 4,000IU being advised.
Interactions with Various Disease States
In persons with both Lupus and Vitamin D deficiency, the normalization of serum Vitamin D to 41.5+/-10.1ng/mL is associated with increased naive and regulatory T cell count and reduced memory B cells, which could possibly be beneficial to Systemic Lupus Erythematosus.
Vitamin D may aid fibromyalgic symptoms (pain and lack of function), but further study is needed. [1]
Vitamin D deficiency may contribute to an age-related loss of muscle function in elderly persons as well as stand as an independent predictor of muscle strength and mass, with lower serum Vitamin D levels being associated with higher risk of Sarcopenia.
Vitamin D supplementation has been associated with preservation of type II muscle fibers in elderly persons and with improved muscular function in Vitamin D deficiency women.
Nutrient Interactions
Safety & Toxicity
Summary
Tldr; Dairy appears to be the best food source for vitamin D3. Cod liver oil effectiveness varies, depending on the processor and the method of analysis. While the previous Recommended Dietary Allowance (RDA) for Vitamin D was adequate to prevent rickets in children, it is now considered insufficient for adults. Research suggests that higher levels of Vitamin D intake are necessary to maintain optimal health in adults.
Various factors such as latitude, skin tone, and environmental conditions can affect the rate of Vitamin D synthesis from sunlight. Of these factors, latitude and skin tone appear to be the most influential.
Those living closer to the equator have a greater ability to produce Vitamin D through sunlight exposure, while individuals with darker skin tones are at a higher risk of Vitamin D deficiency. In fact, it has been observed that areas located above latitude 42.2°N, such as Boston, fail to produce any UVB-induced previtamin D from November to February, a period of four months. This deficiency in Vitamin D synthesis is further prolonged to six months above latitude 55°N, as observed in Edmonton. However, regions located within the range of 18-32°N still produce Vitamin D during the winter.
Sunscreen is able to significantly diminish synthesis of vitamin D, and chronic usage may be associated with vitamin D deficiency, if no oral supplementation exists.
Vitamin D3, also called cholecalciferol, is the common supplement for vitamin D. It is better absorbed compared to other forms of vitamin D.
The activation of Vitamin D3 into its hormone form involves either two stages (if starting from a dietary supplement containing Vitamin D3) or three stages (if starting from skin stores). The skin initiates the first (non-supplemental) conversion, while the liver and kidneys mediate the later two metabolic steps.
Both vitamin D2 and D3 can be used as supplements to increase circulating levels of the active hormone. While some studies suggest that D3 is more effective than D2, others argue that the potency difference can be normalized by standardizing to an IU value.
There is conflicting evidence regarding the effectiveness of vitamin D2 and D3 when compared on an IU basis. Some studies have found them to be bioequivalent, while others suggest a superiority of vitamin D3. However, there are no studies suggesting that D2 is more effective than D3. As a result, it is recommended to choose D3 supplementation.
There are differences in the synthesis and stability of D2 and D3, which are two forms of vitamin D used for supplementation. D3 is synthesized differently from D2 and is more stable than D2 in powder form.
Recommended levels of vitamin D are roughly 75nmol/L (30ng/mL) for some conditions.
Deficiency rates in the population appear to have increased over the past two decades but they may have stabilized in recent years.
Although latitude is a significant factor, it is important to note that vitamin D deficiency (defined by serum levels of 25nmol/L or below) and insufficiency (50nmol/L), are prevalent globally.
In general, a dose of 2,000 IU is sufficient to fulfill the vitamin D needs of most individuals. Doses ranging from 2,000-10,000 IU may not provide any additional benefits, but are not considered toxic either.
Regarding dosing, lower oral doses appear to be more effective in increasing serum vitamin D levels than higher doses, which may have reduced absorption. This variability between individuals suggests that different doses may be needed to achieve the desired level of serum vitamin D. At lower ranges of oral dosing, vitamin D seems to have a linear effect on serum levels, with each 100IU increasing serum by approximately 1-2nmol/L. For instance, 1,000IU is implicated in the range of 10-25nmol/L and 2,000IU in the range of 20-50nmol/L.
Vitamin D is best absorbed with a meal, preferrably one with a little fat in it.
Toxicity has been noted at very high _daily_ doses of vitamin D, which are about 10-fold higher than the aforementioned 2,000IU daily dose.
Vitamin D3 appears to be a more reliable form of supplemental vitamin D, relative to D2, for increasing serum levels to an adequate range.
Several observational studies have reported a negative association between serum vitamin D levels and all-cause mortality.
Clinical trials investigating the impact of vitamin D supplementation on mortality rates have suggested a small reduction in all-cause mortality, particularly in older adults.
Vitamin D3 supplementation appears to be the most efficient form of supplementation for reducing mortality.
It is possible that vitamin D might serve as a biomarker for another factor that is related to longevity. However, there is currently no evidence to suggest that vitamin D supplementation can increase lifespan directly. Rather, it appears that supplementation may indirectly reduce the risk of premature death.
In vitro and animal data suggest that vitamin D can modulate a subset of calcium channels on neurons and regulate cell death through excitotoxicity.
There is evidence of an inverse relationship between vitamin D levels in the blood and symptoms of depression in certain groups.
Multiple Sclerosis (MS) prevalence is correlated with latitude and sun exposure, both of which are in turn correlated with vitamin D levels.
There does appear to be some, albeit weaker, correlation between Alzheimer’s disease and vitamin D.
Low serum vitamin D is correlated with increased risk of Parkinson’s Disease (PD) and further associated with the severity of the disease state.
Observational studies have indicated that low vitamin D levels are linked to an increased risk of cardiovascular disease.
Vitamin D levels have been inversely correlated with insulin resistance and insulin sensitivity in non-diabetic adults.
Daily supplementation of 4000IU appears to lead to improved performance in athletes along with muscle recovery after damage induced by eccentric exercise. A correlation between low Vitamin D levels, illness and athletic injuries appears to exist, especially in regards to stress fractures.
Vitamin D acting upon its receptor does promote mineralization of bone tissue and is correlated with less risk for fractures in the youth. Specifically, vitamin D supplementation appears to further protect individuals from stress fractures.
Vitamin D in serum appears to be positively correlated with overall androgen status, with sufficient levels of vitamin D acting to normalize testosterone. There is currently no evidence to suggest supraphysiological levels of vitamin D further enhances testosterone.
Vitamin D in serum appears to be inversely related to breast cancer risk (higher serum levels being associated with lower risk).
Furthermore, Vitamin D deficiency appears to be more prevalent in persons with diagnosed breast cancer and is similarly correlated with severity of breast cancer. 400-800IU daily appears to be inadequate to decrease the risk of breast cancer, whereas women supplementing with 2000IU of Vitamin D daily, may see up to a 50% reduction in the incidence of breast cancer.
Evidence suggests that even though 1000IU per day is somewhat effective in improving Vitamin D status, a weekly administration of 50,000IU is more effective.
Vitamin D appears to be inversely correlated with risk of colon and colorectal cancers, as well as with Prostate and Ovarian cancer.
For colorectal cancer outcomes, a reduction was observed with 2000IU of supplemental Vitamin D. Additionally, doses as low as 600IU/d lower the risk of pancreatic cancer.
Higher serum Vitamin D appears to be associated with improved lung function as assessed by forced exhalation.
Low levels of Vitamin D are associated with increased corticosteroid use in asthmatic children while supplementation of 1200IU daily is associated with decreased asthmatic attacks in children previously diagnosed with Asthma.
Children taking 1200IU of Vitamin D daily are 40% less likely to get the flu during the winter and supplementing with Vitamin D will help prevent the flu on adults.
Vitamin D also appears to be correlated with sleep quality.
Mechanistically, vitamin D appears to act on the sperm itself (mature spermatid) and improve its motility while enhancing cell survival. 25-50ng/mL (62.4-124.8nmol/L) appears to be an adequate range to preserve optimal seminal properties in otherwise healthy men.
Research suggests that pregnant women have lower serum vitamin D levels compared to non-pregnant women, and this deficiency can have adverse effects on both the mother and the child.
The deficiency is particularly critical during the first trimester, and therefore, supplementing vitamin D only after pregnancy notification may not be the best approach as it may miss the time-sensitive period.
A slightly higher intake of vitamin D may be required to reach sufficiency in pregnant women, relative to nonpregnant women and men, with intakes of up to 4,000IU being advised.
Vitamin D is potentially synergistic with Vitamin K supplementation as the two share many mechanisms of action in the cardiovascular and bone metabolism systems and people with mean serum levels of 86.5 nmol/L had 65% better absorption of calcium than people with mean serum levels of 50 nmol/L.